The EOB is a statement that shows healthcare services you received, the amount paid by your health plan, and any amount you owe to a doctor or other provider.
You can see all your EOBs in your InTouch account. They’re also available in the MyPacificSource app:
Go paperless
In addition to the online version, we also send EOBs by mail. But you can choose not to receive these—helping to cut clutter and save trees.
Log in to InTouch, then go to Profile > Communication Preferences.
How to read your explanation of benefits
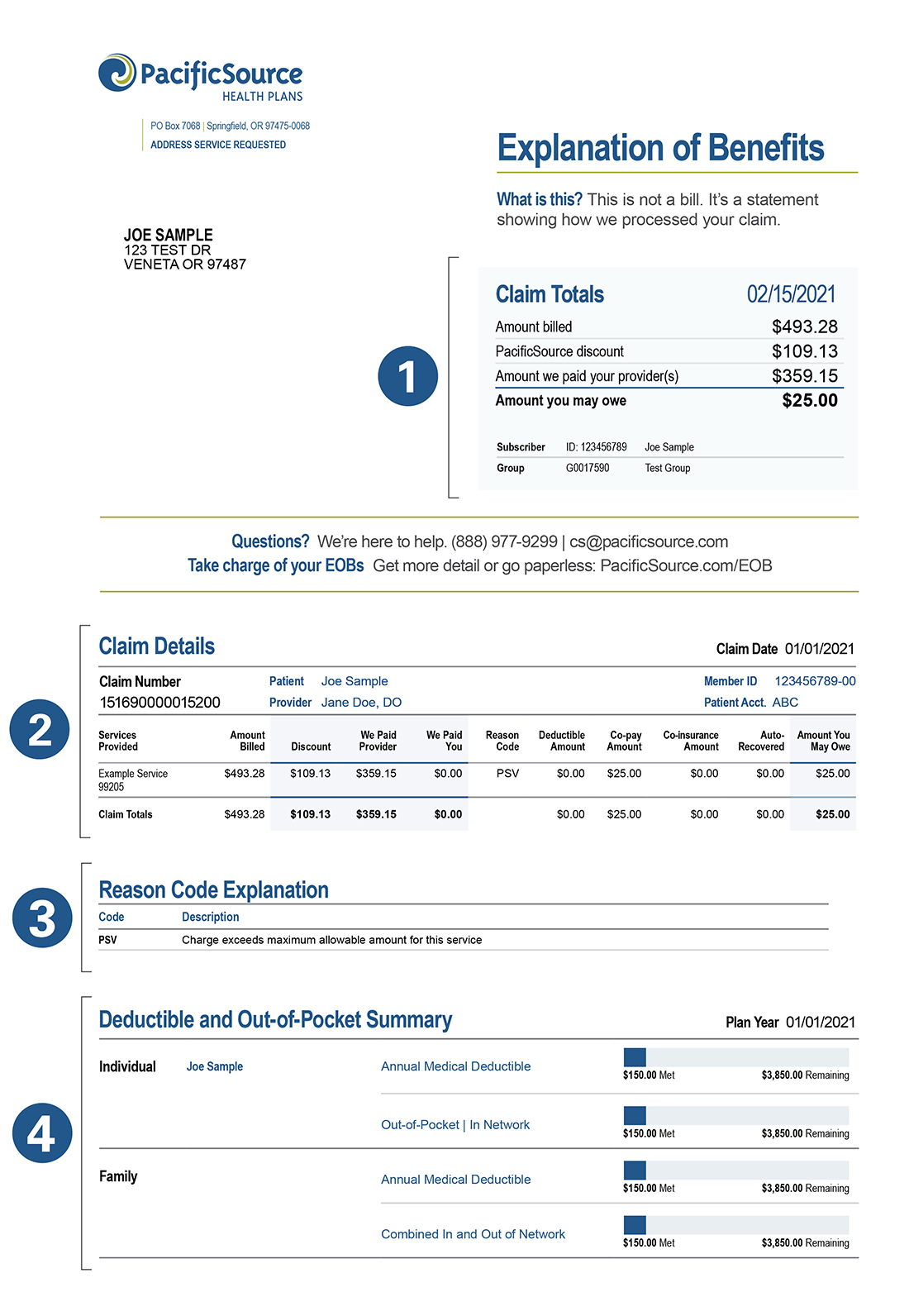
The sections of your EOB
1. Statement Summary
This includes:
- Totals dollar amounts your doctor(s) billed PacificSource for services provided to you or a covered family member
- Amounts paid to your providers
- Cost-sharing amounts, such as copays, coinsurance, or deductibles
2. Claim Details
EOBs sent by mail will consolidate claims for a three-week period, so you may see multiple claims here.
This section includes:
- The date the service was received
- The service provided. Providers assign a code for each service they perform, so you may see several service codes for the same visit.
- The amount billed for the claim
- How your benefits covered the claim. “Discount” is the reduction in your cost if the provider is in your plan’s network.
3. Reason Code Explanations
This section explains why we processed the claim as we did. Here are a few reasons a claim might not be paid as expected:
- We may need more information from you or your provider.
- Your provider's charge for a service may exceed our allowed amount. This is more likely if you visited a provider who is not in your PacificSource network.
- The service may not be covered by your plan.
- You may have exceeded your plan's limit for a particular service.
4. Deductible and Out-of-Pocket Summary
This section shows you:
- How much of your plan's deductible you've met this year. The deductible is the amount you owe for healthcare services before your plan begins to pay.
- Some plans have both a per-member deductible and a per-family deductible.
- Some plans have a separate deductible for out-of-network providers.
- The amount you have paid, year-to-date, for healthcare services.
- Your plan’s out-of-pocket maximums. This is the most you are expected to paybefore your plan pays 100% of the allowed amount.
Totals in this section are based on claims processed through the date on the EOB.